The L.A. Times recently ran an article on the rising increase of dog bites that are sending record numbers of us to local Emergency Rooms. The numbers are actually quite troublesome.
A recent study cited 48,596 ER visits that were related to dog bites, a number that reflects a 12% increase from the previous year and 70% higher than 2005. That equates to 125 ER visits for dog bites per 100,000 California residents.
Why the increase?
As many a 45% of American households now have at least 1 dog. That number is higher than it’s ever been owing to the large number of adoptions that took place during the pandemic when people were suffering from isolation.
Some dogs, like people, respond to unusual stress with aggressive behavior but unfortunately, the initial warning signs may go unnoticed. According to the article, a large number of puppies (and adult dogs as well) were hastily adopted during the pandemic and never properly socialized which has resulted in unaddressed behavioral issues.
State figures and a recent study by public health researchers show that, in California, children and young adults are the age groups most likely to make ER visits for dog bites.
The most serious injuries often involve the head and neck, making little children especially vulnerable. Nationwide, children under 5 were more than twice as likely to die from dog bites as members of other age groups.
What to look for?
Canine aggression occurs “on a ladder” of escalating behaviors and not all of them are obvious unless you know what to look for.
Easy to remember are the 5 Fs:
- fret
- fidget
- fight
- flight
- freeze
Initial signs of discomfort also might include lip-licking, looking away, or yawning. The behavior starts to escalate when the dog begins stiffening up, staring, or crouching with a tucked tail. And things can worsen if an active toddler or small child gets too handsy.

According to Elizabeth Stelow, chief of the Behavior Service at the UC Davis Veterinary Medical Teaching Hospital, owners should learn to recognize anxiety in dogs and understand their body language. When dogs owners repeatedly miss the signs of distress, biting may occur.
Dogs who are punished regularly are also more inclined to bite. Negative feedback such as collars that deliver electronic stimulation, choke chains, and/or pronged collars were also identified in the article as another source of great stress.
Although aversive techniques appear to work by subduing the animal’s behavior, that result is often deceptive. Fear-based learning can push dogs to stop engaging in any behavior, good or bad, as the dog becomes fearful of a negative response.
The American Veterinary Society of Animal Behavior encourages owners to focus on positive reinforcement, rewarding dogs for what they do right. Motivating good behavior with treats, toys, verbal praise, and other positive choices make for a much happier and better-behaved pet.
Be sensitive to any signs that might lead to aggressive behavior.
Dogs are such an important part of our family, our lives, and our wellbeing. Let’s make sure that we equally value the wellbeing of our canine friends.







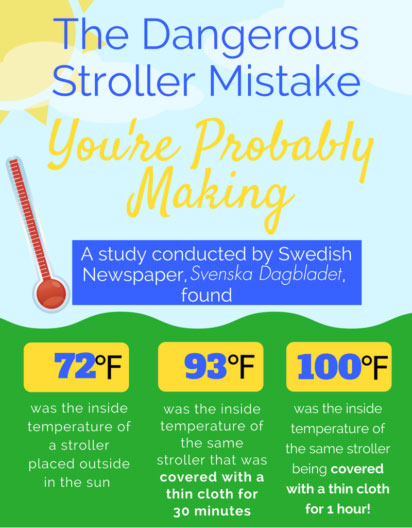 Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!
Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!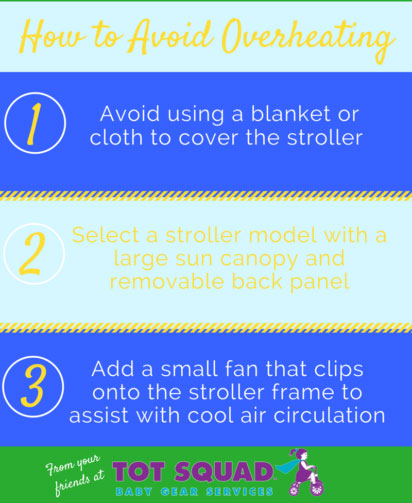 Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.
Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.