When little Enora Lavenir’s parents put her down for a nap during a family vacation they never could have imagined it would result in her death. Vacationing in a Florida Airbnb, the couple didn’t know that the rental home had been a “party house” where the illicit drug Fentanyl had likely been used. Yet, confirmed by autopsy, Enora’s death was due to acute Fentanyl toxicity.
Until now, our perception of the opioid crisis has largely been viewed as an adult problem. However, there is stunning and alarming evidence that infants and children are more likely to die from an opioid overdose than from any other toxic substance.
According to findings published in the journal Pediatrics about 52% of poisoning deaths in children under 5 years of age are due to opioids. “In fact, the number has doubled since 2005, when 24% of poisonings were attributable to opioids” said lead researcher Dr. Christopher Gaw, a pediatric emergency physician at Childrens Hospital of Philadelphia.
Dr. Gaw and colleagues reviewed child death data from the U.S. National Center for Fatality Review and Prevention. Between 2005-2018, 731 poisoning deaths in children aged 5 and younger were reported to the center. Overall, infants, under the age of 1 accounted for 2/5 (40%) of poisoning deaths. During this period opioids were involved in 47% of these deaths. The next leading cause of drug related deaths occurred from over the counter pain & cold medications (15%).
Five years later, the numbers are rising.
Even a small dose of a prescription opioid can put an infant or toddler’s life at risk. This is particularly true of synthetic opioids such as Fentanyl which is 50-100 times more potent than morphine.

Where are these overdose deaths occurring?
Nearly 2/3 of these poisoning deaths occur in the infant or child’s home. Roughly 1/3 of these occurred when a child was supervised by someone other than their parents. The data clearly shows that the vast majority of these poisonings were accidental. Dr. Gaw added “Kids are curious, active and we know from experience and other studies that often kids are exposed accidentally. They are just exploring their environment when they find an opioid and end up ingesting it. A lot of these are what we call exploratory ingestions.”
Dr. Sam Wang, a pediatric toxicologist with Childrens Hospital Colorado in Aurora noted ”even legitimate opioids that are not properly stored and kept out of reach of a child can cause a death if a child would get into them.” On the other hand, illicit drugs are particularly risky in homes where supervision of children is usually not as good. This type of event is considered drug endangerment. Our readers need to understand that, even when properly prescribed opioids are in the home, they must be stored safely – away from little ones.

SIGNS OF AN OPIATE OVERDOSE:
- Very lethargic, hard to arouse
- Shallow, slower breathing
- “Pinpoint” pupils
If any of these occur call 9-1-1 immediately and if breathing stops, initiate CPR immediately
Our Pediatric CPR & Family Safety Class begins with a focus on prevention of most household injuries & accidents.
When it comes to storing any potentially dangerous drugs we emphasize:
- storing all medication (prescription or otherwise) out of the reach of children
- keeping opioid drugs under lock and key, if possible
- that medications of this type be kept in child resistant containers
Consider asking you M.D. for a prescription for Naloxone, the proven life-saving antidote to all opiate drugs.




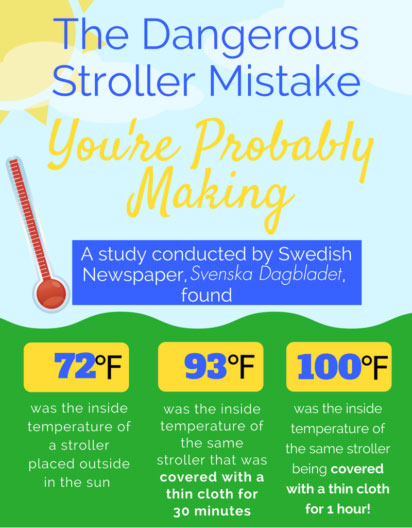 Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!
Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!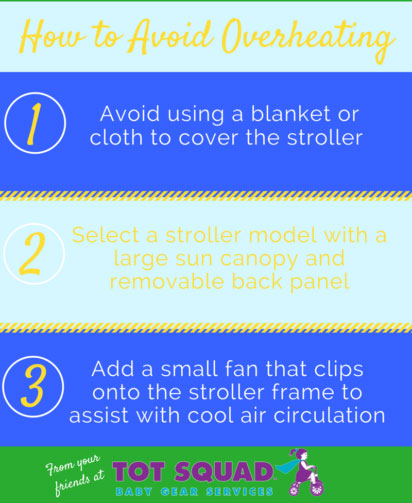 Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.
Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.