Hype or hyperbole? Headlines scare people, for sure. The number of coronavirus comments, articles and statistics can make you shudder. You might even purchase protective masks or simply stay home in fear.
Americans, much like many others, are actually at much greater risk from a virus which is here, now. This season, influenza (the Flu), has already claimed the lives of at least 40 children and it remains a far greater health concern for your family than any other communicable disease.
According to the Centers for Disease Control & Prevention (CDC) the flu has sickened 13 million Americans this winter, putting 120,000 of them in the hospital and has already taken 6,600 lives. The flu season has not yet peaked and when all data is in the flu may take as many as 61,000 American lives.
Protection from the flu takes a number of forms. Although imperfect due to the changing nature of viral illnesses, the flu vaccine is still your best hedge against this awful disease. According to the CDC, fewer than half of American adults got a flu shot last season. For children, who are more vulnerable to the respiratory effects of the flu, only 62% received the vaccine last year.
Dr. Paul Offit, director of the Vaccine Education Center at Children’s Hospital of Philadelphia believes that because the exotic viruses from foreign lands have such different and scary names (Ebola, Zika, Wuhan, etc.) we fear them even more than our generic annual flu strains. When the SARS virus caught our attention, causing a global panic, the U.S. “dodged a bullet” according to the CDC with only 8 Americans becoming infected. There were no deaths from SARS in the U.S. Yet, it caused panic on a global scale.
Children are most often hit the hardest with the flu and statistics reveal that most kids who die from the flu virus have not been immunized against it. Many of these children were previously healthy.
Protection from the flu not only includes getting vaccinated. If you or a family member develops a fever, body aches, headache and/or cough they should be seen by the family physician and screened as early as possible for the flu. Early detection is essential as there are anti-viral medications that can be prescribed to lessen the negative impact.
Other simple methods of disease prevention include keeping sick individuals at home, frequent hand washing and covering ones mouth when coughing.

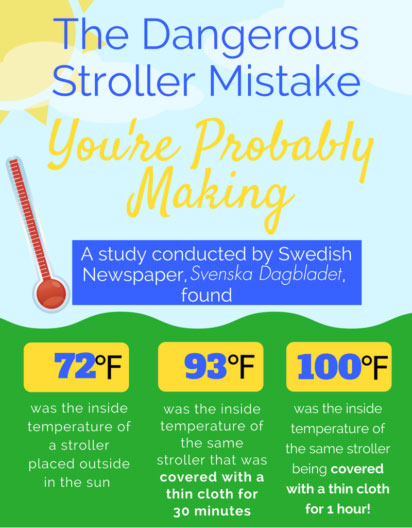 Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!
Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!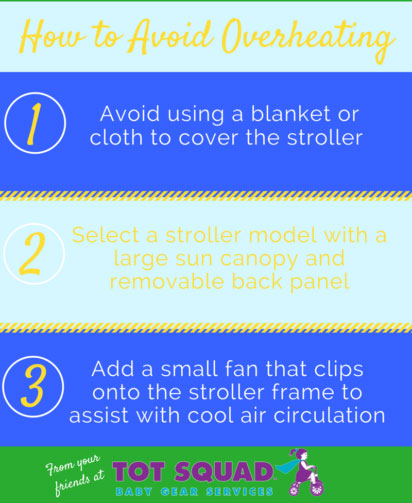 Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.
Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.