The American Academy of Pediatrics (AAP) wants parents to know that sleeping in their car seats when not in transport has significant risk and has caused an alarming number of deaths nationwide.
Dr. Jeffrey Colvin, the lead author of a study looking at risk for infants in car seats, found that “most of the deaths occurred when the car seat was being used as a sleeping device.” He further noted “It really appears that the deaths in these car seats occurred in the context where the car seat wasn’t being used for its purpose in transporting a child, but instead it was being used as a substitute for a crib or bassinet.”
The AAP study further noted that “compared with other deaths, deaths in sitting devices had higher odds of occurring under the supervision of a child care provider or babysitter (our italics) compared with a parent.”
Dr. Colvin told Today that while there is no definitive reason for the number of deaths in car seats, he suggested the angled position of the device might be a factor, as well as the straps and side padding that could potentially be a strangulation or suffocation risk. He also stressed that “before there is widespread panic every time a child falls asleep in a car seat, parents should absolutely not be concerned if their baby falls asleep during the usual time in transit.” Various experts have opinions as to how long it is safe for them to be sleeping during a car trip. Please discuss this with your pediatrician for their expert advice.

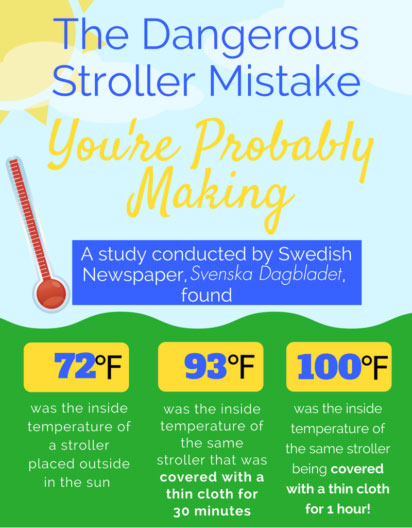 Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!
Based on an interview with Stockholm pediatrician Dr. Svante Norgren about the dangers of covering a stroller, the Swedish newspaper, Svenska Dagbladet, conducted an experiment by putting a stroller out in the sun, midday, in the summer. Without a cover, the stroller was about 72 degrees Fahrenheit. After covering the stroller with a thin cover for 30 minutes, the temperature rose to 93 degrees and after an hour, 100 degrees!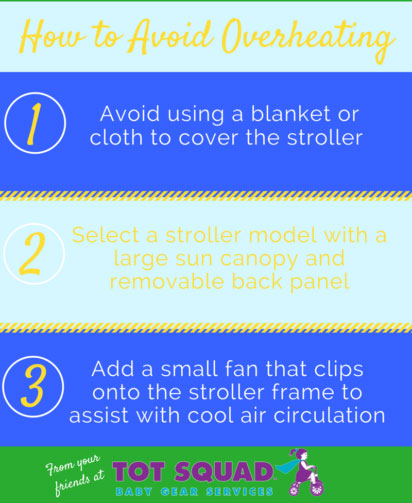 Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.
Dress children lightly, use plenty of sunscreen, and keep them well-hydrated. Sponge your child with a damp cloth to keep them comfortable. A small clip-on fan can be attached to their stroller for added circulation – just be sure to keep it out of reach.